BME Faculty Rapidly Engage in COVID-19 Research
Collaborations are key for BME researchers pivoting to address COVID-19.
by Eric Laine
When the emerging global coronavirus pandemic began disrupting teaching and research activities in the Spring 2020 semester, the Meinig School of Biomedical Engineering faculty responded with collaborative research projects and entrepreneurial endeavors focused on attacking the problem from multiple angles.
In May 2020, Cornell’s Office of the Vice Provost for Research (OVPR) launched the Rapid Research Response SARS-CoV-2 Seed Grant program to fund preliminary investigations into medical and biological aspects of the virus that causes COVID-19. The program aims to invest in innovative research ideas to address this critical global need and generate preliminary data for future research grant applications.
Cornell BME was ready to play a leading role in finding effective solutions through a broad range of research into key aspects of the problem, from diagnosing the virus, to developing therapeutic strategies, and ultimately working toward a vaccine. Many such efforts are now being supported by the seed grant funding.
“It’s very, very possible that something that comes out of these grants will have a direct impact in the crisis we are trying to solve,” said Emmanuel Giannelis, vice provost for research and the Walter R. Read Professor of Engineering, about the seed grant program.
Multi-domain Experts
Cornell BME faculty are well-positioned to address the COVID-19 problem. “It’s not a shift in focus, but a natural extension of our faculty expertise,“ said Marjolein van der Meulen, the James M. and Marsha McCormick Director and Swanson Professor of Biomedical Engineering. BME labs were already working on the kinds of projects that are most needed now, so applying the work to COVID-19 is a natural fit.
“Biomedical engineers are multi-domain experts,” said Professor Newton de Faria, director of the Meinig School’s Master of Engineering (M.Eng.) program. The discipline demands knowledge in disease state fundamentals such as anatomy, physiology, pathophysiology and mechanisms of action, as well as the various engineering approaches employed to produce solutions, such as fluid dynamics, sensors and actuators, modeling, automation and control.
In addition to research, BME faculty are using the pandemic topic in classroom and lab instruction to focus student attention on how biomedical engineers develop and apply solutions to emerging medical needs. The scope of BME presents a range of opportunities for collaboration with other departments and fields of research, and with business and industry.
“Collaborations are essential for each one of the projects,” said van der Meulen. “The seed grants provide the opportunity to start collaborative projects, collect data and then apply to other funding agencies such as NIH for further support.”
Addressing Patient Care
Assistant Professor Ilana Brito is working with Elmhurst Hospital Center in New York City, whose physicians are witnessing steep increases in bacterial superinfections in patients with COVID-19 upon admission. These bacterial superinfections may be indicative of significant morbidity and mortality when associated with SARS-CoV-2.
Using computational analysis, Brito’s team has found molecular evidence for how bacteria interact with human cells. These data suggest that the dangers of SARS-CoV-2 infection may not be limited to those caused by the virus itself.
They hypothesize that the interaction between SARS-CoV-2, the immune system and the human respiratory tract microbiome may contribute to the severity of COVID-19 infections. These interactions may also serve as prognostic indicators and, importantly, may indicate whether patients with COVID-19 should be treated with certain antibiotics.
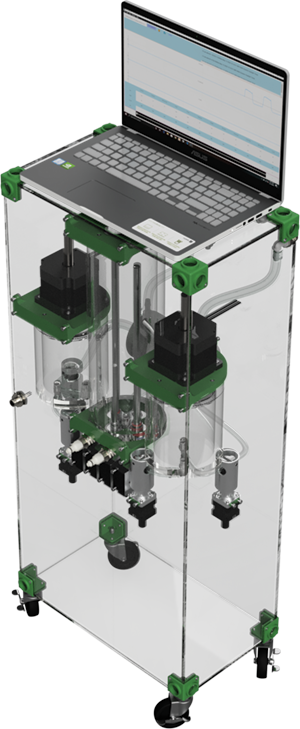
Other investigations into patient care are focused on devices. Dr. Kamal S. Turkmany from Weill Cornell Medicine – Department of surgery, received a Weill Cornell Medicine Clinical and Translational Science Center award to work on a new ventilator design to help improve outcomes of COVID-19 patients requiring assisted mechanical breathing.
Patients with severe COVID-19 can develop acute respiratory distress syndrome (ARDS) and because of the delicate nature of this condition, air/ oxygen gas ventilators have not been as effective as expected.
In response, Dr. Turkmany, collaborating primarily with Professor Newton de Faria, is developing a total liquid ventilator device. “Liquid ventilation has been extensively studied and has some advantages compared to gas ventilation,” de Faria said, “including anti-inflammatory properties and clearing of secretions and debris.”
The liquid ventilator project was conceived by Dr. Turkmany and relies on collaboration with researchers from the Cornell College of Veterinary Medicine, the School of Electrical and Computer Engineering, and the Lewis Katz School of Medicine at Temple University.
The team has had to overcome new challenges arising from the work restrictions imposed by the pandemic response. “Navigating the justified but complex processes to gain access to labs, procurement and exchange of materials and components, and the inability of being physically present, continue to be deterrents,” de Faria said. “We have been industrious and have been able to move our project forward.”
A Multi-Antigen Vaccine
Professor David Putnam, working in collaboration with Matthew DeLisa, the William L. Lewis Professor of Engineering in the Smith School of Chemical and Biomolecular Engineering, submitted a winning SARS-CoV-2 Seed Grant proposal to make a multi-antigen vaccine against the virus.
The roots of this collaboration go back more than 10 years, as Putnam and DeLisa have worked together to design and develop vaccines based on engineered bacterial outer membrane vesicles (rOMVs), flexible, controllable nanoparticles that can be modified for use in a wide array of applications.
Their team successfully developed a universal vaccine against influenza that is now moving toward Phase 1 human clinical trials through a $17.9 million contract from the National Institutes of Health to Versatope Therapeutics, Inc., which was founded to bring this vaccine to the market. Putnam and DeLisa now turn their attention to designing and developing a multi-antigen vaccine against SARS-CoV-2.
A single antigen vaccine works well if the immune response to that specific antigen, such as a protein, sugar or peptide, is known to prevent infection. So far, Putnam said, “no one knows what antigen will induce protective immunity,” for SARS-CoV-2 infection. “Therefore, a shotgun approach is needed wherein we make a best guess of what antigens could lead to protection and box them up into a vaccine. It mimics the virus to the best of our ability.”
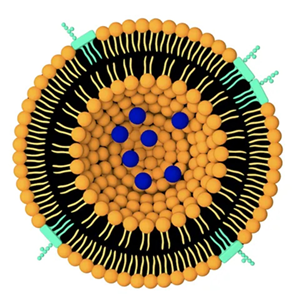
Putnam and DeLisa’s seed grant proposal is focused on the design of multi-antigen rOMV-based vaccines. “The working hypothesis is that multi-antigen rOMV vaccines will better mimic the antigenic composition of the SARS-CoV-2 virus and enhance the probability of a functional vaccine,” the proposal states.
A multi-antigen vaccine has an additional benefit over a single antigen vaccine. If the virus mutates, the mutation usually occurs in one of the antigens. A multivalent vaccine will still protect the patient.
Putnam has high praise for his CBE colleague, and he deems the collaboration essential. “Matt is an expert in engineering bacteria,” Putnam said. “Without him, my lab would not be working in the microbiology field at all.” The partnership ensures expertise in all areas of vaccine production, from vector design, formulation and immune response, to antigen expression and characterization.
“To develop a vaccine you need biologists, epidemiologists, computational scientists, immunologists, clinicians, pharmaceutical chemists, bioprocess engineers, business development, finance experts, regulatory experts and others,” Putnam said. “BME students are trained in each of these areas. We can speak the language across these disciplines, and communication is the key to product development.”
The funding provided through the seed grant program will allow the team to purchase reagents necessary for the multitude of sequential tasks in the process, and subsidize the work of graduate students for the project. Phase 2 funding will focus on evaluating induced passive immunity using infection mouse models of SARS-CoV-2 in development elsewhere within Cornell's research community.
A Liquid Biopsy for COVID-19
Iwijn De Vlaminck, assistant professor, was another BME recipient of a SARS-CoV-2 Seed Grant. His team’s proposal received funding to develop and assess the utility of a blood test designed not to detect infection, but to identify and quantify injury to internal organs and tissues.
While COVID-19 primarily affects the lungs, evidence is emerging of a more systemic disease involving multiple organs. Clinicians and researchers around the world are reporting heart muscle inflammation as well as irregular heart rhythms, neurological damage including brain inflammation and seizures, and kidney damage. De Vlaminck’s blood test would look for markers that would indicate which organs have been affected.
“We do this by quantifying the tissues of origin of circulating cell-free DNA in blood,” De Vlaminck said. “Cell-free DNA are short fragments of DNA that freely circulate in blood. These molecules are the remnants of dead cells.”
The genomes of these dead cells remain in the patient’s bloodstream for some time. De Vlaminck’s team developed a technique to quantify the cell, organ and tissue types from which these free-floating molecules are derived. It profiles specific epigenetic markers comprised in cell-free DNA using DNA sequencing-based approaches.
“This technique enables a ‘liquid biopsy’ for COVID-19,” De Vlaminck explained. “We can quantify the degree of injury to any organ or tissue with a molecular, minimally invasive blood test. Such a test could help identify patients at high risk of disease, and also help to clarify the multi-organ involvement of COVID-19.”
The blood test would also indicate the degree of injury to a particular organ by revealing the amount of cell-free DNA derived from that organ. This measure would allow physicians to monitor the injury of infected patients to assess disease severity and the efficacy of applied therapies.
De Vlaminck’s work on this project is based on patient samples and clinical materials that would not be accessible without physician collaborators. The team has worked closely with researchers at the University of California San Francisco, McGill University and the Dana Farber Cancer Institute. These collaborations enabled them to assess the utility of their test with two independent groups of COVID-19 patients.

The team is using the seed grant funding to support materials and services expenses related to DNA sequencing, which carries a cost of approximately $500 per sample. Multiple samples from multiple patients are needed in each phase of the project. This initial grant positions the team well to pursue external funding for expanded efforts.
“The seed grant allowed us to undertake a risky project quickly,” De Vlaminck said. “There are numerous external funding opportunities for this type of work, but the funding cycles are slow. The seed grant mechanism enabled us to move forward.”
The OVPR Seed Grants were meant to get researchers working on COVID-19-related projects as quickly as possible to allow investigators to generate preliminary data needed to apply for additional funding. For Cornell BME researchers, the plan is working.

